Written by Bernie Carr
I posted earlier that I was admitted to the hospital when my COVID-19 symptoms took a turn for the worst.
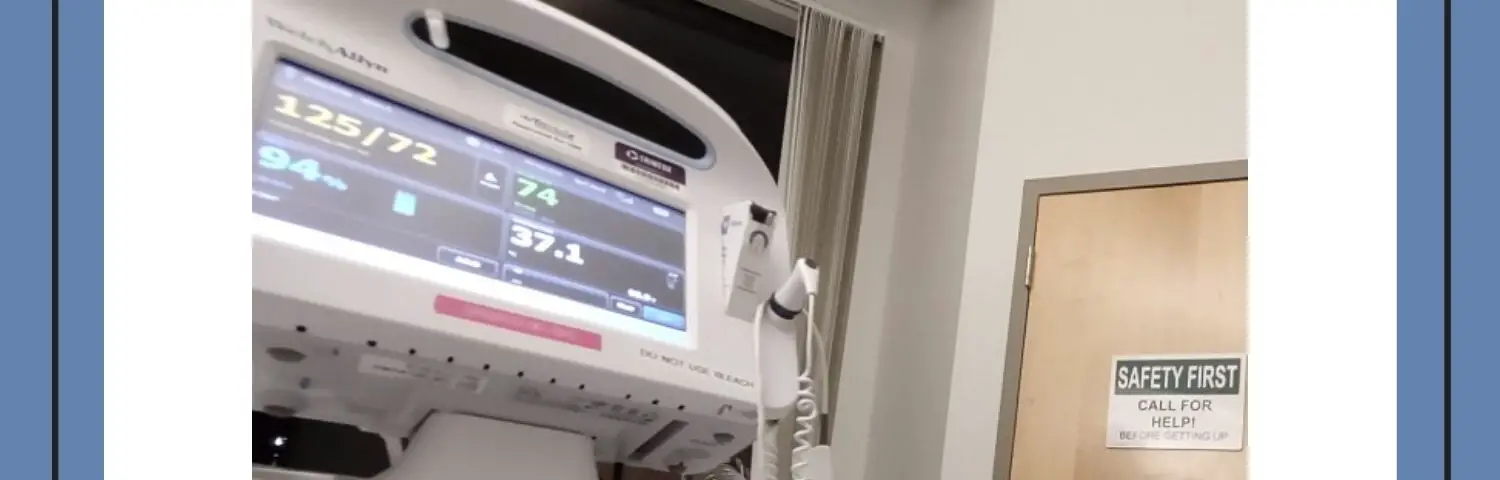
After a couple of hours in the Emergency Department, I was moved to a hospital room. I was on oxygen the whole time. Just getting out of the bed to use the bathroom was a major undertaking. I would rapidly lose oxygen in a short amount of time.
I was admitted at night, and the next morning I was in for a lot of tests. I had a chest X-ray, chest MRI, several blood draws, the whole time hooked up to oxygen.
My oxygen level dropped again and the nurses took action and reported it to the physician. I was then switched to a “high flow oxygen” machine because the regular oxygen was not enough. Because of this, I was moved to a Intermediate Care Room. It is one level above a regular room, but one level below an Intensive Care Unit (ICU).
At this point, I was in a world of uncertainty about my condition. The doctors were also concerned about blood clots occurring in the chest and lungs. Finally, I got separate visits from teams of doctors: Infectious Disease, Pulmonary and Attending doctor. They all told me the diagnosis: COVID-19 pneumonia.
What is COVID-19 pneumonia?
The way one of the doctors explained it to me, most COVID-19 cases turn out mild and the person recovers quickly. But in some cases, COVID-19 gets into your lungs and wreaks havoc. It causes inflammation and damages the air sacs within the lungs. They then get filled with fluid, making it difficult to breathe.
Unfortunately, this is what happened to me. I was told that this can happen to anyone, even someone who does not have any underlying medical issues. So much is still unknown about COVID-19, they cannot predict whose genetic makeup may be susceptible to this.
I am not a medical professional, so I can only rely on what I was told at the hospital.
As far as treatment, the doctors recommended IV antibiotics, steroids, blood thinners, and many other medications, I can’t name them all. I had to be monitored constantly and nurses came in every hour to check vital signs: blood pressure, temperature, pulse and of course, oxygen level. They drew blood daily, usually around 3 am. With so many blood draws, I felt I was running out of available veins to draw on; they had to keep poking around to search.
The priority was to get me in a stable condition and I was willing to try the necessary tests and treatments. I needed all the prayers and help I could get. I was still in a precarious situation as doctors were concerned about blood clots developing.
Progress
After three days, I was relieved to find out there were no blood clots found, and my lungs were stable. By the fourth day, I felt a marked improvement – I could actually eat better and did not feel as miserable as in previous days. I thank God for the progress.
The next goal was to get off the high flow oxygen and get into regular oxygen. The doctor even mentioned that patients who cannot move off high flow oxygen get moved to a rehab facility after the hospital stay. That was something I did not want to do.
A couple of days later, I was finally able to function on regular oxygen and off the high flow oxygen.
Discharge
After a week and a day, I was discharged. The staff arranged for an oxygen tank to be sent home with me, along with an oxygen machine which was delivered after I got home.
My oxygen levels taken with the pulse oximeter still goes down with any activity, even just writing this blog. I have to rest constantly to get oxygen levels back up. I have a follow up visit scheduled with a Pulmonologist in a couple of weeks.
I asked the doctors at the hospital how long does it take for lungs to heal and they told me it varies among individuals and there is no way to tell how long the process will take. They all said COVID-pneumonia causes lung damage and scarring.
I went from being an active person who exercises daily to someone who has trouble catching a breath after walking a few steps. They encouraged me to keep doing the hourly breathing exercises they taught me at the hospital using a spirometer. I do these breathing exercises on a regular basis.
COVID-19 Pneumonia: What to watch for
Some signs to watch for that COVID-19 is causing pneumonia:
- shortness of breath
- rapid breathing
- rapid heartbeat
- dizziness
- sweating
Risk factors include: over age 65, diabetes, obesity, asthma, lung disease, heart disease, liver disease or renal failure. However, I did not have any of these risk factors, yet I still caught it.
When to seek emergency care
According to the CDC, go get emergency care if you notice the following:
- Trouble breathing
- Persistent pain or pressure in the chest
- New confusion
- Inability to wake or stay awake
- Pale, gray, or blue-colored skin, lips, or nail beds, depending on skin tone
The bottom line
I am glad I went to the Emergency Room when I experienced shortness of breath. If I hadn’t, I’d have gotten a lot worse. It was tough being in isolation at the hospital but the medical and nursing staff all treated me with utmost kindness and compassion. If you experience COVID-19 worsening symptoms, get medical help right away.
For the next article in the series, see What’s It Like Being on Oxygen?
The final article in the series: I Got Off Supplemental Oxygen
June 22 is Prime Day! Please consider helping out the blog by clicking on our Amazon links. We are an affiliate of Amazon.com, which means we received a small commission if you click through one of our Amazon links when you shop, at totally no cost to you. This helps keep the lights on at the blog. Thanks!
Prime Day Lead Up Deals: Amazon HomeAbout the author:
Bernie Carr is the founder of Apartment Prepper. She has written several books including the best-selling Prepper’s Pocket Guide, Jake and Miller’s Big Adventure, The Penny-Pinching Prepper and How to Prepare for Most Emergencies on a $50 a Month Budget. Her work appears in sites such as the Allstate Blog and Clark.com, as well as print magazines such as Backwoods Survival Guide and Prepper Survival Guide. She has been featured in national publications such as Fox Business and Popular Mechanics. Learn more about Bernie here.

Here’s hoping you heal up quickly Bernie. We need you.
Hi Joseph, Thanks for the kind words, nice to be needed 🙂 I really appreciate it.